Dealing with Diabetes
The Nita Family Opens Up and Shares How Community Involvement and Digital Health Helps Families Deal with Type 1 Diabetes
Imagine waking up one morning to find your child going into diabetic ketoacidosis — a life-threatening complication from diabetes. Blood flow slows throughout your child’s body as your child slips in and out of consciousness, barely able to move. You head to the hospital, where all your child can do is blink his/her eyes to signal yes or no to questions from doctors.
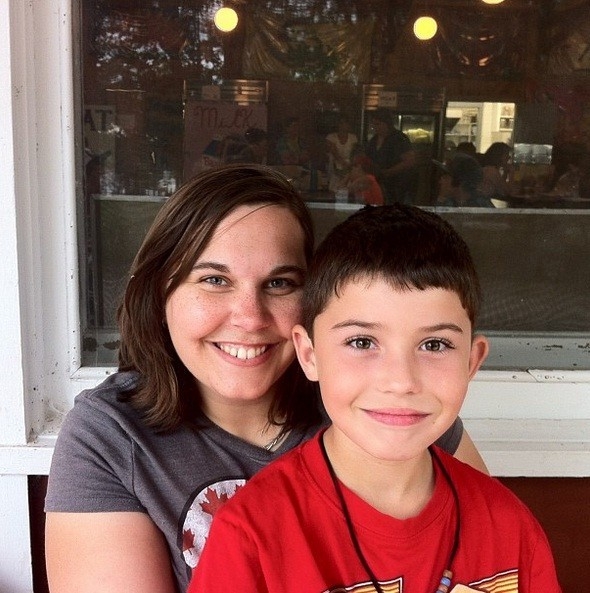
This is how Sara Nita, 31, found her child Marcus, 8, on a September morning three years ago.
“He said, ‘No one gave this to me. God gave this to me and I intend to find out why.’ And that sent me into a complete meltdown,” recalls Sara.
Type 1 diabetes is a disease where the pancreas does not produce any insulin. Insulin is a hormone used to control the amount of sugar in the blood. It repurposes the sugar and uses it as energy. Without insulin, sugar builds up in the blood and results in life- threatening consequences.
“Before Marcus was diagnosed, he didn’t even like chips or pop or candy or anything,” says Sara. “I used to think he was the worst possible kid this could happen to because he was always so healthy.”
Unfortunately, there are no preventable measures to take when it comes to Type 1 diabetes and the cause remains unknown. However, according to the Canadian Diabetes Association, it is believed Type 1 diabetes occurs because the body’s immune system destroys insulin-producing cells.
Once diagnosed, the battle with Type 1 diabetes is lifelong — there is currently no cure. The only option is to manage and monitor blood sugar levels. This may not seem like the be-all and end-all, but for an eight-year-old child, it turns the world upside down.
“It was rough,” says Sara about Marcus’ diagnosis. “All of a sudden he had to take on all of this responsibility.”
Marcus wakes up in the morning and immediately washes his hands to check his blood sugar levels. He pokes himself with a lancing device and uses a drop of blood on a test strip. The blood sugar meter generates a number corresponding with his levels, which he then enters in his insulin pump. The pump releases the correct amount of insulin to keep his blood sugar levels steady.
Meal times mean more work. At breakfast, lunch, snack time and dinner, Marcus must do more checks. He must also enter the number of carbohydrates he ingests every time he eats so the insulin pump can balance his levels. This means Marcus is extremely knowledgeable about the food he consumes.
“When it comes to food, Marcus can look at the plate and know exactly how many carbohydrates are on it,” says Sara. “He cares about what he consumes. He has become the food police at home!”
A day is not complete without some type of physical activity, meaning more monitoring. When Marcus is active, such as playing soccer or going to the park, he needs insulin to produce energy.
Every 20 minutes he must check his levels to make sure he is getting the insulin he needs.
Even with all of the checking, double-checking and constant monitoring, it is hard to always remain within the target zone for blood sugar levels.
“I feel bad because I feel like his childhood is robbed,” says Sara. “Growing up, when I was a kid, I could go outside and run around until dark. But with Marcus, he can’t. He has to check in every so often and make sure we know his blood sugar numbers.”
Some days are easier than others. Bad days may include feeling low on energy, mood swings and not being able to participate in all activities.
“Originally, Marcus was okay with having diabetes,” says Sara. “But now he hates it. He is slowly forgetting to do things at school for his disease and by the time he gets home, he doesn’t feel great. There’s no point in scolding him.”
But these times are not only tough on Marcus; Sara feels defeated too.
“There are going to be many people in his life that can eat whatever they want, just like I can,” Sara says. “But Marcus will always point out how it isn’t fair. He will say, ‘I wish you had it.’ And I just tell him I wish I could take the diabetes from him.”
Luckily Sara found a way to help make the entire process, including the bad days, more manageable.
A digital health tool, connects Sara and Marcus to all the help they need. The Better Health Together, by Canada Health Infoway, features the stories of Canadians who are using digital health tools.
Sara and Marcus can digitally keep track of Marcus’ numbers, creating better organization. Marcus’ health- care providers have access to these numbers and can see how he is doing on a regular basis. During bad times, the health-care providers have immediate access to Marcus’ data and can provide emergency diagnosis and treatment.
“We can upload Marcus’ pump data and email it off instead of sitting on the phone for hours and making sure the numbers are all correct,” says Sara. “It’s fantastic.”
Sara says using a digital health tool not only cuts out the middle step of having to pass along information through a long chain of people, but also allows Marcus to be more actively involved in a disease that will affect him for the rest of his life.
“Although Marcus is only eight-years-old, it’s his diabetes,” says Sara. “And the fact is I’m not going to be around forever. I try to keep him informed about what we do and why we do it.”
For now, Sara says digital health tools are making her life simpler.
“The technology helps us to work with our doctors. Diabetes is 24 hours a day, seven days a week. It never ends,” says Sara. “Digital health is making it easier to get help whenever we need it.”
The Better Health Together campaign demonstrates there is a wide range of families with medical needs. Testimonials on the campaign’s web site prove digital health is making a difference. Here are a few other examples.
Cheryl says digital medical records reduce the time she spends explaining her daughter’s medical history, making more efficient appointments.
Cathy uses digital health to reduce partial or miscommunication between health-care providers. It helps pass on all of the important information.
Allison says on-line health tools give her resources to find emotional support when she is having a difficult time with her family’s health.
Other forms of digital technology are also making a difference for the Nita family. Sara says she often turns to Twitter to find answers to her questions.
“I found the whole on-line diabetes community,” says Sara. “Even the smallest answer from anywhere in the world makes you feel better. They helped me get through my slump.”
Sara and Marcus are also members of Juvenile Diabetes Research Founda- tion (JDRF), a global leader in finding a cure to Type 1 diabetes through research funding and advocacy. JDRF provides information on how to live to the fullest while dealing with diabetes. Through events such as the Telus Walk to Cure Diabetes and the Ride for Diabetes Research, JDRF is a group of people coming together for a common cause.
“Marcus can mostly do whatever he wants. He gets to be a kid, but he just has to take insulin to keep him alive,” explains Sara. “Right now it is a life- saver, but it isn’t a cure.”
Three years after Marcus’ initial diagnosis of Type 1 diabetes, the Nita family tries to focus on the positive and finds escapes when needed.
“As a family we like to go geocaching or we go to the movies,” says Sara. “We try to do a lot of family things to put the diabetes thing out of our minds. It doesn’t define us.”








